
Smoking Impacts on Lung.

Smoking has significant and harmful effects on the respiratory system and the body as a whole. Here's an overview of what happens to the lungs after smoking and the positive changes that occur when you quit:
Effects of Smoking on the Lungs:

Tar Buildup:
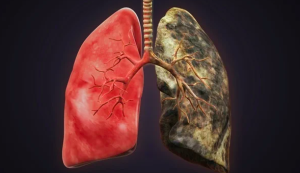
The term "tar" refers to the sticky, brown residue that is left behind in the lungs and airways when tobacco is smoked. This substance is a complex mixture of chemicals, including carcinogens (cancer-causing substances), and it is a major contributor to the negative effects of smoking on the lungs. Here's how tar buildup affects the lungs:
Deposition in Airways:
When tobacco is burned, tar is released and inhaled into the lungs along with other smoke constituents. The tar contains numerous toxic substances, including polycyclic aromatic hydrocarbons (PAHs) and other chemicals.
Airway Obstruction:
Tar can accumulate on the walls of the bronchi and bronchioles, which are the large and small air passages in the lungs. Over time, this buildup can lead to the narrowing of the airways, making it more difficult for air to flow freely during breathing.
Reduced Lung Function:
The presence of tar in the lungs contributes to chronic inflammation and irritation. This can lead to conditions such as chronic bronchitis, where the airways are inflamed and produce excess mucus, further obstructing airflow. Reduced lung function is a hallmark of chronic obstructive pulmonary disease (COPD), which includes conditions like chronic bronchitis and emphysema.
Alveolar Damage:
Tar can also reach the alveoli, the tiny air sacs in the lungs where oxygen exchange takes place. The deposition of tar in the alveoli can cause damage and interfere with the exchange of oxygen and carbon dioxide.
Increased Risk of Respiratory Infections:
The presence of tar and other toxic substances in the lungs weakens the immune system's defenses, making individuals more susceptible to respiratory infections like pneumonia and bronchitis.
Cancer Risk:
Many of the chemicals in tar are known carcinogens, and long-term exposure increases the risk of developing lung cancer. Tar contributes to the formation of cancerous cells in the lung tissue.
Environmental Advantages of Recycling Plastics.
Bronchoconstriction:

Bronchoconstriction refers to the narrowing of the air passages (bronchi and bronchioles) in the lungs. inhaling smoke has a direct impact on the respiratory system, leading to irritation and inflammation of the airways, which, in turn, can result in bronchoconstriction. Here's how inhale smoke affects the lungs in terms of bronchoconstriction:
Irritation and Inflammation:
The chemicals present in cigarette smoke, including nicotine and various irritants, can irritate the lining of the airways. This irritation triggers an inflammatory response as the body attempts to defend itself against the perceived threat.
Smooth Muscle Constriction:
In response to the inflammation, the smooth muscle surrounding the airways may contract, leading to bronchoconstriction. This narrowing of the air passages makes it more difficult for air to flow in and out of the lungs, particularly during exhalation.
Increased Mucus Production:
Smoking also stimulates the production of excess mucus in the airways. The combination of bronchoconstriction and increased mucus can further obstruct the air passages, making breathing more challenging.
Chronic Bronchitis:
Long-term exposure to cigarette smoke can contribute to chronic bronchitis, a condition characterized by persistent inflammation of the bronchi and increased production of mucus. This chronic irritation and inflammation contribute to the narrowing of the airways.
Reduced Lung Function:
Bronchoconstriction, inflammation, and increased mucus production collectively lead to reduced lung function. This impairment in lung function is a key feature of chronic obstructive pulmonary disease (COPD), a progressive and debilitating respiratory condition associated with inhaling smoke.
Exacerbation of Asthma:
For individuals with asthma, inhaling smoke can exacerbate bronchoconstriction and worsen asthma symptoms. The combination of smoking and asthma can lead to more frequent and severe asthma attacks.
Increased Risk of Respiratory Infections:
The compromised airways are more susceptible to respiratory infections. Smoking weakens the immune system's ability to defend against infections, leading to an increased risk of conditions such as pneumonia and bronchitis.
Reduced Ciliary Function:
Cilia are tiny hair-like structures found in the respiratory tract, including the bronchi and bronchioles, that play a crucial role in maintaining the health of the lungs. The coordinated movement of cilia helps to move mucus, along with trapped particles and microorganisms, out of the respiratory system. Smoking has detrimental effects on ciliary function, and here's how:
Paralysis and Damage:
The chemicals in cigarette smoke can damage and paralyze the cilia. Over the long run, this harm impedes the cilia's capacity to move in an organized way, diminishing their viability in cleaning bodily fluid and particles off of the aviation routes.
Increased Mucus Retention:
With reduced ciliary function, mucus produced in the airways is not efficiently cleared. This prompts an amassing of bodily fluid, which can add to aviation route hindrance and increase the gamble of respiratory diseases.
Risk of Chronic Bronchitis:
The impaired clearance of mucus due to reduced ciliary function contributes to the development of chronic bronchitis. Chronic bronchitis is characterized by persistent inflammation of the bronchi and increased mucus production.
Susceptibility to Infections:
Cilia assume a pivotal part in safeguarding against respiratory contaminations by assisting with eliminating microorganisms and trash. When ciliary function is compromised, the lungs become more susceptible to infections such as pneumonia and bronchitis.
COPD Progression:
Chronic obstructive pulmonary disease (COPD), a condition that includes chronic bronchitis and emphysema, is associated with long-term smoking. Reduced ciliary function contributes to the progression of COPD by allowing inflammation and mucus buildup to persist in the airways.
Slower Recovery from Respiratory Illnesses:
Smokers may experience a slower recovery from respiratory illnesses due to compromised ciliary function. The disabled capacity to clear bodily fluid can drag out side effects and increase the seriousness of respiratory diseases.
Inflammation and Infection:
Smoking has significant and harmful effects on the lungs, particularly in terms of inflammation and increased susceptibility to respiratory infections. Here's how inhaling smoke affects the lungs in terms of inflammation and infection:
Chronic Inflammation:
Smoking leads to chronic inflammation in the airways and lung tissue. The inhalation of toxic chemicals from cigarette smoke triggers an immune response, causing the release of inflammatory mediators. Prolonged inflammation contributes to tissue damage and structural changes in the lungs.
Airway Remodeling:
Chronic inflammation can lead to structural changes in the airways, a process known as airway remodeling. This remodeling may result in the thickening of airway walls, increased mucus production, and narrowing of the air passages. These changes contribute to airflow limitation and reduced lung function.
Reduced Immune Response:
Smoking weakens the immune system's ability to respond effectively to infections. The function of immune cells in the lungs, such as macrophages and neutrophils, is compromised by exposure to cigarette smoke. This impaired immune response makes individuals more susceptible to respiratory infections.
Increased Risk of Respiratory Infections:
Smokers are at a higher risk of developing respiratory infections, including acute bronchitis, chronic bronchitis, and pneumonia. The combination of reduced ciliary function, impaired immune response, and chronic inflammation creates an environment conducive to bacterial and viral infections.
Exacerbation of Chronic Respiratory Conditions:
For individuals with pre-existing respiratory conditions such as asthma or chronic obstructive pulmonary disease (COPD), smoking can exacerbate inflammation and worsen symptoms. This can lead to more frequent and severe episodes of wheezing, coughing, and shortness of breath.
Impaired Wound Healing:
Smoking hinders the process of wound healing in the lungs. The chronic inflammatory state created by inhaling smoke can interfere with the repair of damaged lung tissue, making it more challenging for the respiratory system to recover from injuries.
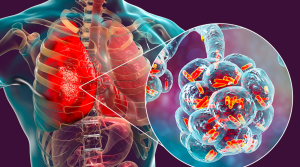
Lung Cancer:
Long-term exposure to cigarette smoke is a major risk factor for lung cancer. The chronic inflammation caused by smoking contributes to the development of cancerous cells in the lung tissue.
Foods that support weight loss.
Emphysema:

Emphysema is a progressive and irreversible lung condition that is often associated with long-term smoking. It is a type of chronic obstructive pulmonary disease (COPD) characterized by damage to the air sacs (alveoli) in the lungs. Smoking is the primary cause of emphysema, and its effects on the lungs contribute to the development and progression of this condition. Here's how inhaling smoke affects the lungs in the context of emphysema:
Alveolar Damage:
Smoking exposes the lungs to harmful chemicals, including irritants and toxins. Over time, chronic exposure to these substances damages the delicate walls of the alveoli, which are responsible for the exchange of oxygen and carbon dioxide in the lungs.
Loss of Elasticity:
The destruction of alveolar walls leads to the loss of elasticity in the lung tissue. Normally, the lungs expand and contract easily during breathing due to the elastic properties of the alveoli. In emphysema, this elasticity is compromised, making it difficult for the lungs to recoil and expel air effectively.
Air Trapping:
Emphysema results in the enlargement of air spaces within the lungs, primarily the alveoli. As a consequence, the air can become trapped in these enlarged spaces during exhalation. This leads to hyperinflation of the lungs and further impairs the ability to expel air, resulting in increased residual volume.
Difficulty Breathing:
The loss of lung elasticity and the destruction of alveoli make it progressively harder for individuals with emphysema to breathe. They may experience shortness of breath, especially during physical exertion, and over time, even simple activities like walking or climbing stairs can become challenging.
Chronic Cough:
Emphysema is often accompanied by chronic bronchitis, another form of COPD. Chronic bronchitis involves persistent inflammation and mucus production in the airways. The combination of emphysema and chronic bronchitis contributes to a chronic cough.
Reduced Exercise Tolerance:
As emphysema advances, individuals may experience a significant decline in exercise tolerance. This is due to impaired lung function, reduced oxygen exchange, and increased work of breathing.
Risk of Respiratory Infections:
Individuals with emphysema are at an increased risk of respiratory infections, such as pneumonia and bronchitis, due to compromised lung defenses and impaired clearance of mucus from the airways.
Positive Changes After Quitting Smoking:

Immediate Improvement:
Quitting smoking brings about immediate improvements to various aspects of health, even within a short period after cessation. Here are some positive changes that occur shortly after quitting smoking:
Improved Oxygen Levels:
Within hours of quitting, carbon monoxide levels in the blood begin to decrease. Carbon monoxide is a toxic gas present in cigarette smoke that competes with oxygen for binding to hemoglobin in red blood cells. As carbon monoxide levels drop, oxygen levels in the blood increase, leading to improved oxygen transport to vital organs and tissues.
Enhanced Lung Function:
The respiratory system starts to recover immediately after quitting. The bronchial tubes begin to relax, and lung function improves. This leads to increased airflow and ease of breathing.
Decreased Heart Rate and Blood Pressure:
Nicotine in cigarettes stimulates the release of adrenaline, which can elevate heart rate and blood pressure. Within the first day of quitting, the heart rate begins to decrease, and blood pressure starts to normalize.
Improved Circulation:
Smoking constricts blood vessels, leading to reduced blood flow. When inhaling smoke is stopped, blood vessels start to relax and widen, enhancing circulation throughout the body. This improved circulation benefits the heart, skin, and other organs.
Lowered Risk of Cardiovascular Events:
Quitting smoking immediately reduces the risk of cardiovascular events such as heart attacks and strokes. The positive changes in blood pressure, heart rate, and circulation contribute to a more heart-healthy state.
Enhanced Sense of Taste and Smell:
Smoking dulls the senses of taste and smell. Within days of quitting, these senses begin to sharpen, allowing individuals to enjoy food more and perceive scents more accurately.
Improved Respiratory Symptoms:

Smokers often experience respiratory symptoms such as coughing and shortness of breath. Within a few weeks of quitting, these symptoms tend to improve as the respiratory system starts to heal.
Reduction in Coughing and Wheezing:
The irritation caused by smoking can lead to chronic coughing and wheezing. After quitting, the airways begin to relax, and the frequency of coughing and wheezing typically decreases.
Better Skin Health:
Smoking accelerates skin aging and contributes to wrinkles. Stopping smoking elevates better bloodstream to the skin, decreasing the presence of kinks and advancing better coloring.
Cilia Functionality:
One of the positive changes that occur after quitting smoking is the improvement in cilia functionality. Cilia are little hair-like designs in the respiratory lot that assume a significant part in keeping up with lung wellbeing. The cilia's fundamental capability is to move bodily fluid and cough particles out of the aviation routes, assisting with safeguarding the lungs from diseases and aggravations. Here's how cilia functionality improves after quitting smoking:
A scientific way to reduce belly fat.
Recovery of Cilia:
Smoking damages and impairs the function of cilia in the airways. The chemicals in cigarette smoke interfere with the normal movement of cilia, reducing their effectiveness in clearing mucus and foreign particles. When a person quits inhaling smoke, the recovery process begins, and cilia gradually regain their ability to move.
Enhanced Mucus Clearance:
As cilia recover, the clearance of mucus from the respiratory tract becomes more efficient. This is important for maintaining a healthy airway environment by removing irritants, microbes, and debris. Improved mucus clearance contributes to a lower risk of respiratory infections.
Reduced Respiratory Irritation:
Cilia play a crucial role in preventing respiratory irritation by clearing away irritants that may otherwise lead to chronic inflammation. As cilia function improves, the risk of persistent irritation and inflammation in the airways decreases.
Lowered Risk of Respiratory Infections:
The recovery of cilia function enhances the lung's defense mechanisms against infections. Productive bodily fluid leeway forestalls the development of irresistible specialists, decreasing the gamble of respiratory contaminations like bronchitis and pneumonia.
Improved Lung Health:
Restoring cilia functionality is a key aspect of overall lung health. Efficient cilia movement contributes to the maintenance of clear and healthy airways, supporting optimal respiratory function.
Reduced Inflammation:
Quitting smoking leads to various positive changes in the body, including a reduction in inflammation. Smoking is a significant reason for ongoing irritation, which is connected to various medical conditions. When a person quits smoking, the body undergoes a series of positive changes that contribute to a decrease in inflammation. Here's how quitting inhaling smoke reduces inflammation:
Lowering Inflammatory Markers:
Smoking is related to expanded degrees of fiery markers in the blood, like C-receptive protein (CRP), and supportive of provocative cytokines. After quitting, these markers tend to decrease, indicating a reduction in systemic inflammation.
https://livewithgreen.com/smoking-impact-on-lungs/
.jpg)